Solar urticaria is a rare condition characterised by an allergic reaction to sunlight, which causes hives or welts on the skin when exposed to sunlight. This guide will help you understand and manage sun-induced skin sensitivity caused by solar urticaria.
Recognizing Solar Urticaria: Signs and Symptoms
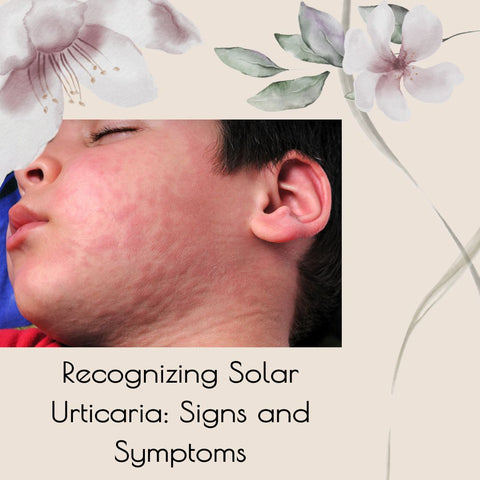
Recognising solar urticaria requires awareness of the signs and symptoms that appear after exposure to sunlight. What to look for includes hives or welts, rash distribution, symptom timing, repeated episodes, systemic symptoms, and photo testing. If you experience hives, welts, or other unusual skin reactions after sun exposure, especially if they occur frequently or are accompanied by systemic symptoms, consult a doctor for an accurate evaluation and diagnosis.
Early Indications of Solar Urticaria: What to Look For
Recognising solar urticaria in its early stages requires awareness of subtle signs and symptoms that could indicate an allergic reaction to sunlight. Here are some early indicators to watch for:
-
Persistent itching or tingling on the skin during or immediately after sun exposure may be an early indicator of solar urticaria. This itching may precede the appearance of hives or welts.
-
Mild redness or erythema on sun-exposed skin, such as the face, neck, arms, or chest, can be an early sign of solar urticaria. This redness may appear soon after sun exposure and worsen with time.
-
Some people may feel warmth or burning on their skin before developing hives or welts. This sensation may be limited to sun-exposed areas and may worsen with continued sun exposure.
-
Localised swelling or edoema in sun-exposed areas of the skin are early indicators of solar urticaria. This swelling may be subtle at first, but it can progress to more pronounced swelling or hives with time.
-
Small, raised bumps or papules may appear on the skin soon after sun exposure, indicating an allergic reaction. These papules may be accompanied by itching or burning, and they can precede the formation of larger hives or welts.
-
Some people may experience tingling or prickling sensations on their skin, similar to "pins and needles," as an early sign of solar urticaria. This sensation may occur before the development of visible skin changes.
-
Early signs of solar urticaria may include increased sensitivity to sunlight, with symptoms worsening with sun exposure. Individuals may notice that their skin reacts more strongly to sunlight than usual, even after a brief exposure.
Differentiating Solar Urticaria from Common Sunburn
Understanding the distinct characteristics of each condition is necessary to distinguish solar urticaria from common sunburn. Here's how to distinguish between them.
Solar Urticaria:
-
Solar urticaria usually manifests as hives or welts on the skin shortly after exposure to sunlight. These raised, red, or white bumps can vary in size and shape and appear abruptly and intensely.
-
Solar urticaria symptoms, such as hives or welts, typically appear within minutes to hours of sun exposure and can last for several hours or days. The reaction may occur quickly and then subside once sun exposure is discontinued.
-
Solar urticaria frequently produces intense itching, burning, or stinging sensations in the affected areas. Individuals may feel discomfort or pain in addition to the appearance of hives or welts.
-
Solar urticaria rash is typically limited to sun-exposed areas of the skin, including the face, neck, arms, and chest. The reaction may be more noticeable in areas directly exposed to sunlight.
-
Solar urticaria may be associated with systemic symptoms such as headache, nausea, dizziness, or fatigue. These symptoms may indicate a more severe allergic reaction, which should be evaluated by a medical professional.
Common sunburn:
-
Sunburn usually appears as red, inflamed skin that feels warm or tender to the touch. Over several hours, the skin may become more red and eventually peel as it heals.
-
Sunburn symptoms, such as redness and discomfort, usually appear several hours after sun exposure and peak between 24 and 48 hours later. Sunburn severity may vary depending on skin type, sun intensity, and exposure duration.
-
Sunburn often causes pain, tenderness, or discomfort in the affected areas, especially when touched or exposed to heat. Individuals may experience a sensation of warmth or burning on the sunburned skin.
-
Sunburn affects areas of the skin that are exposed to sunlight, such as the face, neck, shoulders, and back. The severity of sunburn may vary depending on the extent of sun exposure and the use of sun protection measures.
-
Sunburn can increase the risk of skin damage, premature aging, and skin cancer over time, especially with repeated or severe sun exposure. It's important to take steps to prevent sunburn and protect the skin from harmful UV radiation.
When to Seek Medical Advice: Solar Urticaria Symptoms
If you have symptoms of solar urticaria or are concerned about your skin's reaction to sunlight, you should see a doctor for an accurate diagnosis and treatment. They can evaluate your symptoms, make an accurate diagnosis, and suggest appropriate treatment to help you manage your condition effectively.
Approaching Treatment: Effective Strategies for Solar Urticaria

Treatment for solar urticaria focuses on symptom management and reducing the allergic reaction to sunlight. Here are some effective ways to treat solar urticaria:
-
Avoidance of Sun Exposure: The primary strategy for treating solar urticaria is to limit exposure to sunlight. This could include staying indoors during peak sunlight hours, wearing protective clothing, hats, and sunglasses, and seeking shade whenever possible.
-
Sunscreen Application: Apply a broad-spectrum sunscreen with a high sun protection factor (SPF) to sun-exposed areas of the skin before going outside. Choose a sunscreen that protects against both UVA and UVB radiation, and reapply it as directed.
-
Phototherapy: Also referred to as light therapy, phototherapy is the controlled application of particular light wavelengths to the skin to desensitise it and lessen the intensity of symptoms associated with solar urticaria. Under the guidance of a dermatologist or allergist with experience treating solar urticaria, phototherapy should be administered.
-
Antihistamines: Medications taken orally to reduce itching, swelling, and hives related to solar urticaria can be helpful. Non-sedating antihistamines such as cetirizine (Zyrtec), loratadine (Claritin), or fexofenadine (Allegra) are commonly used to manage symptoms.
-
Topical Steroids: To lessen inflammation and soothe itching brought on by solar urticaria, doctors may prescribe topical corticosteroid creams or ointments. These drugs should only be used under a doctor's supervision and are applied directly to the skin's afflicted areas.
-
EpiPen or other epinephrine autoinjectors: Those who have experienced severe allergic reactions or anaphylaxis in the past may need to carry an epipen. This is an emergency drug that you can give yourself if you have a severe allergic reaction to sunlight.
-
Immunomodulatory Therapy: In certain cases, patients with severe solar urticaria may be prescribed immunomodulatory drugs, such as omalizumab (Xolair), to lessen their immune system's reaction to sunlight and avoid allergic reactions.
-
Allergen Immunotherapy: If other treatments are ineffective for a patient's severe solar urticaria, allergen immunotherapy—also referred to as allergy shots—may be a possibility. The goal of this therapy is to gradually desensitise the immune system to sunlight over time by carefully regulating exposure.
-
Skin Care: To relieve and shield the skin impacted by solar urticaria, use mild skin care products. Use mild, fragrance-free cleansers and moisturizers, avoid harsh soaps or skincare products, and pat the skin dry gently after bathing to minimize irritation.
-
Consultation with Specialists: See a dermatologist or allergist for specialised evaluation and management if over-the-counter remedies are ineffective or if solar urticaria severely affects your quality of life. These experts can provide personalised treatment recommendations based on your unique requirements and medical background.
It's important to work closely with a healthcare professional to develop a comprehensive treatment plan for solar urticaria based on your symptoms, triggers, and medical history. Many people with solar urticaria can effectively control their symptoms and improve their quality of life by following proper management and sun protection measures.
First-Line Treatments: Antihistamines and Their Role
Antihistamines help to manage the symptoms of solar urticaria by blocking histamine and relieving itching, swelling, and hives. Individual responses to antihistamine therapy may vary, and some people may require additional treatments or combination therapy to achieve optimal symptom control. Working closely with a healthcare professional is essential for developing a comprehensive treatment plan that is tailored to your specific needs and medical history.
Advanced Options: Exploring Phototherapy and Immunotherapy
For people with solar urticaria who do not respond well to first-line treatments like antihistamines, advanced options like phototherapy and immunotherapy may be considered. Let us take a closer look at these treatment options:
Phototherapy (Light Therapy):
-
Phototherapy, also known as light therapy, involves controlled exposure to specific wavelengths of light to desensitize the skin and reduce the severity of solar urticaria symptoms. The goal is to gradually increase tolerance to sunlight over time.
-
Several types of phototherapy may be used to treat solar urticaria, including narrowband UVB (NB-UVB) therapy, UVA1 therapy, and PUVA therapy (psoralen plus UVA). These treatments vary in the wavelength of light used and the duration and frequency of exposure.
-
Phototherapy sessions are typically conducted under the supervision of a dermatologist or allergist experienced in treating solar urticaria. The duration and frequency of treatment sessions are gradually increased based on the individual's response and tolerance to light exposure.
-
Phototherapy is effective in reducing the severity and frequency of solar urticaria symptoms in some individuals. However, the response to phototherapy may vary, and multiple sessions may be required to achieve optimal results.
-
Side effects of phototherapy may include skin irritation, redness, and increased sensitivity to sunlight. It's essential to discuss potential risks and benefits with a healthcare professional before starting phototherapy treatment.
Immunotherapy:
-
Immunotherapy, also known as allergen immunotherapy or desensitization therapy, aims to modulate the immune system's response to sunlight allergens and reduce the severity of allergic reactions in individuals with solar urticaria.
-
There is limited research on the use of immunotherapy for solar urticaria, but it may involve the administration of gradually increasing doses of sunlight allergens through subcutaneous injections or sublingual tablets. This helps desensitize the immune system to sunlight exposure over time.
-
Immunotherapy for solar urticaria is typically conducted under the supervision of an allergist or immunologist experienced in treating allergic conditions. The treatment protocol may vary based on the individual's response and tolerance to immunotherapy.
-
The efficacy of immunotherapy for solar urticaria is still being studied, and more research is needed to determine its effectiveness. Some studies have reported promising results in reducing the severity and frequency of solar urticaria symptoms in some individuals.
-
Side effects of immunotherapy may include local reactions at the injection site, allergic reactions, and systemic symptoms. It's essential to discuss potential risks and benefits with a healthcare professional before starting immunotherapy treatment.
DIY Care: Home Remedies and Preventative Measures
While professional medical advice is required for managing solar urticaria, some home remedies and preventative measures may help alleviate symptoms and reduce the likelihood of flare-ups. Here are a few DIY care tips:
Home Remedies for Relief:
-
Apply a cool compress or cold pack to the affected areas to relieve itching and inflammation. Wrap the compress in a thin cloth to avoid direct contact with the skin, then apply it for 10-15 minutes at a time.
-
A lukewarm bath with colloidal oatmeal can help relieve the itching and irritation caused by solar urticaria. Soak for 15-20 minutes in bathwater with colloidal oatmeal. Next, gently pat the skin dry.
-
Apply pure aloe vera gel to the affected areas to relieve inflammation, reduce redness, and promote healing. Aloe vera's natural anti-inflammatory and moisturising properties can help relieve solar urticaria symptoms.
-
Make a paste of baking soda and water and apply it to hives or welts to relieve itching and irritation. Leave the paste on for 10-15 minutes before rinsing with warm water.
-
Apply calamine lotion to the affected areas to relieve itching and discomfort caused by solar urticaria. Calamine lotion is a cooling agent that can help dry out hives or welts.
Preventative Measures:
-
Reduce sun exposure, especially during peak hours (typically between 10 a.m. and 4 p.m.). Wear protective clothing, wide-brimmed hats, and sunglasses to protect your skin from direct sunlight.
-
Before going outside, apply a broad-spectrum, high-SPF sunscreen to all exposed skin. Reapply sunscreen every two hours, or more often if swimming or sweating. Select a sunscreen that is suitable for sensitive skin and protects against both UVA and UVB rays.
-
Seek shade whenever possible, especially during the hottest part of the day, midday. Use umbrellas, trees, or awnings to provide shade and reduce direct sunlight exposure.
-
Protect yourself from the sun by wearing lightweight, breathable clothing that covers your skin. Choose loose-fitting, light-colored fabrics that reflect sunlight rather than absorb it.
-
Stay hydrated by drinking plenty of water throughout the day, especially if you spend time outside in hot weather. Proper hydration promotes skin health and lowers the likelihood of dehydration-related symptoms.
-
Identify and avoid known triggers or allergens that can worsen solar urticaria symptoms. Keep a diary to track flare-ups and identify patterns of sun exposure or other possible triggers.
-
Gentle skincare involves using mild, fragrance-free cleansers and moisturisers that are appropriate for sensitive skin. Avoid using harsh soaps, hot water, or excessive scrubbing, as these can irritate the skin and exacerbate symptoms.
Prevention and Lifestyle: Living with Solar Urticaria

Living with solar urticaria necessitates careful management and lifestyle changes to alleviate symptoms and improve quality of life. Here are some preventative and lifestyle tips for people with solar urticaria:
Prevention Strategies:
-
Stay indoors during peak sunlight hours, which are typically 10 a.m. to 4 p.m. When going outside, wear protective clothing, wide-brimmed hats, and sunglasses to protect your skin from direct sunlight.
-
Apply a broad-spectrum sunscreen with a high sun protection factor (SPF) to all exposed skin before going outside. Reapply sunscreen every two hours or more frequently if swimming or sweating.
-
Seek shade whenever possible, especially at midday when the sun's rays are strongest. Use umbrellas, trees, or awnings to provide shade and reduce direct sunlight exposure.
-
To protect yourself from the sun, wear light, breathable clothing that covers your skin. Choose loose-fitting, light-colored fabrics that reflect rather than absorb sunlight.
-
Stay hydrated by drinking plenty of water throughout the day, especially if you spend time outside in hot weather. Proper hydration promotes skin health and lowers the risk of dehydration-induced symptoms.
-
Identify and avoid known triggers or allergens that can worsen solar urticaria symptoms. Keep a diary to track flare-ups and identify patterns of sun exposure or other possible triggers.
Lifestyle Adjustments:
-
To avoid sun exposure during peak sunlight hours, opt for indoor or shaded activities. Choose early morning or late afternoon outdoor activities when the sun's rays are less intense.
-
Use cool compresses, cold packs, or fans to relieve itching and discomfort during flare-ups. Taking cool showers or baths may also provide relief from symptoms.
-
Tanning beds and sunlamps should be avoided because they can cause or exacerbate solar urticaria. Artificial UV radiation can be just as harmful as natural sunlight.
-
To help manage stress, try stress-reduction techniques like mindfulness, meditation, deep breathing exercises, and yoga. Stress can exacerbate solar urticaria symptoms, so it is important to find ways to relax and unwind.
-
Use gentle skincare products that are suitable for sensitive skin, and avoid harsh soaps, hot water, and excessive scrubbing, which can irritate the skin and worsen symptoms.
-
Consider wearing a medical alert bracelet or carrying an identification card that shows you have solar urticaria. This can be useful in the event of a severe allergic reaction or an emergency requiring medical attention.
-
Seek support from friends, family, or online communities that understand your situation and can offer encouragement and understanding. Sharing experiences and coping strategies with others who have solar urticaria can be beneficial.
Sun Safety Tips: Protective Measures for Sensitive Skin
Individuals with sensitive skin must practise sun safety to avoid sunburn, skin damage, and other negative reactions to sunlight. Here are some protective measures and sun safety tips designed specifically for sensitive skin:
Sunscreen Selection:
-
Choose a broad-spectrum sunscreen that protects against UVA and UVB rays. Look for "broad-spectrum" products to ensure complete sun protection.
-
Choose physical or mineral sunscreens with zinc oxide or titanium dioxide, which sit on top of the skin and reflect UV rays away from it. These ingredients are less likely to irritate sensitive skin than chemical sunscreens.
-
Choose sunscreen formulations that are fragrance-free and designed for sensitive skin. Fragrances and other additives may irritate sensitive skin and cause allergic reactions.
-
Look for sunscreens that are hypoallergenic or designed for sensitive skin. These formulations are less likely to contain common allergens and are recommended for people with sensitive skin.
-
Choose water-resistant sunscreens, particularly if you plan to sweat or swim. Water-resistant formulas offer longer-lasting protection and are less likely to wash away with perspiration or water exposure.
-
Wear lightweight, long-sleeved shirts, pants, and skirts made from tightly woven fabrics to provide additional protection against UV radiation. Choose clothing with UPF (Ultraviolet Protection Factor) labels for enhanced sun protection.
-
Wear wide-brimmed hats or caps with brims that provide shade to the face, ears, and neck. Opt for hats made from breathable fabrics such as cotton or linen for added comfort.
-
Protect your eyes from UV radiation by wearing sunglasses with UV-blocking lenses. Look for sunglasses labeled as providing 100% UV protection to shield your eyes from harmful rays.
By following these sun safety tips and protective measures, individuals with sensitive skin can enjoy outdoor activities while minimizing the risk of sunburn, skin damage, and other adverse reactions to sunlight. To preserve skin health and lower the chance of developing long-term sun-related skin problems, sun protection must be given top priority all year round, not just during the summer.
The Role of Diet and Nutrition in Managing Solar Urticaria
A healthy diet and the inclusion of specific nutrients may help support overall skin health and potentially reduce inflammation associated with solar urticaria, even though there is no one diet or nutritional plan that can cure the condition. Here's how nutrition and diet can help control solar urticaria:
Anti-Inflammatory Foods:
-
Omega-3 Fatty Acids: Include foods high in omega-3 fatty acids, such as fatty fish (salmon, mackerel, sardines), flaxseeds, chia seeds, and walnuts. Omega-3 fatty acids have anti-inflammatory properties and may help reduce the inflammation caused by solar urticaria.
-
Antioxidant-Rich Foods: Include fruits (berries, oranges, grapes), vegetables (spinach, kale, broccoli), nuts, seeds, and green tea in your daily diet. Antioxidants protect the skin from oxidative stress and may improve immune function.
-
Vitamin C: Consume foods rich in vitamin C, such as kiwis, strawberries, citrus fruits, and bell peppers. A potent antioxidant, vitamin C enhances the production of collagen and maintains the health of the skin.
-
Vitamin E: Include foods high in this nutrient, such as avocados, spinach, sunflower seeds, and almonds. Vitamin E may have anti-inflammatory properties and aids in shielding the skin from UV ray damage.
Hydration:
-
Water: To stay hydrated, drink enough water throughout the day. Staying properly hydrated promotes the body's natural detoxification processes and helps preserve the health of the skin.
-
Herbal Teas: In addition to being hydrating, herbal teas like chamomile, green tea, and rooibos tea also contain antioxidants that may be good for your skin.
Potential Triggers:
-
Identify Food Triggers: Some people with solar urticaria may experience an increase in symptoms after eating certain foods or additives. Keep a food diary to track your diet and any potential links to symptom flare-ups.
-
Food Sensitivities: If you suspect that certain foods are causing or exacerbating your symptoms, speak with a healthcare professional or registered dietitian about possible food sensitivities or intolerances.
Adapting Your Daily Routine: Strategies for Minimizing Exposure
Adapting your daily routine to reduce sunlight exposure is critical for managing solar urticaria. Here are some strategies to help you reduce sun exposure and lower the risk of flare-ups:
-
Schedule outdoor activities in the early morning or late afternoon, when the sun is less intense. To avoid sun exposure during the middle of the day, engage in indoor activities. Consider exercising indoors at a gym or fitness centre, or taking indoor exercise classes. Stay active indoors by engaging in hobbies or activities that do not require direct sunlight.
-
To avoid direct sun exposure, spend your time outside in shaded areas such as covered patios, shaded parks, or outdoor cafes with umbrellas. Wear lightweight, long-sleeved shirts, trousers and wide-brimmed hats to protect as much skin as possible. To get more sun protection, wear clothing made of tightly woven fabrics.
-
Use a broad-spectrum sunscreen with a high SPF on all exposed skin, including the face, neck, ears, and hands. Reapply sunscreen every two hours, or more often if swimming or sweating. Wear sunglasses with UV-blocking lenses to shield your eyes from harmful UV radiation. To protect your lips from sun damage, apply a lip balm with SPF.
-
When travelling, opt for transportation options with shaded seating or enclosed cabins, such as trains, buses, or cars with tinted windows. Avoid open-air vehicles or modes of transportation that have been exposed to direct sunlight for an extended period. When walking or cycling outside, plan your route to include shaded areas or tree-lined streets to reduce direct sun exposure.
-
Create shaded outdoor spaces in your home or workplace using umbrellas, awnings, or shade sails. Design outdoor areas with natural shade from trees or shrubs for added protection. Consider installing UV-protective window films or shades to reduce UV radiation exposure indoors while still allowing natural light.
-
Plan outdoor activities during early morning or late afternoon hours when the sun's rays are less intense. Limit time spent outdoors during peak sunlight hours between 10 a.m. and 4 p.m. Check the UV index forecast before planning outdoor activities. Avoid outdoor activities when the UV index is high, as this indicates an increased risk of sunburn and UV radiation exposure.
-
If sunlight exposure is a concern in your workplace, consider discussing accommodations with your employer, such as adjusting work hours, providing shaded outdoor break areas, or allowing flexible scheduling options. If your job requires outdoor work, use protective equipment such as wide-brimmed hats, sunglasses, long-sleeved clothing, and sunscreen to minimize sun exposure.
Broadening the Horizon: Beyond Immediate Management
Beyond immediate treatment, people with solar urticaria can look into other ways to improve their overall well-being and quality of life. Here are some broader perspectives to consider:
-
Stress management, regular exercise, and healthy sleeping habits are all components of holistic health.
-
Emotional support is provided through support networks as well as therapy or counselling.
-
Career and work-life balance adjustments, as well as social activities, are examples of lifestyle adaptations.
-
Education and advocacy include educational resources and advocacy efforts.
-
Long-term planning includes regular medical checkups and treatment advances.
People with solar urticaria can address not only the physical symptoms but also the lifestyle and emotional aspects of having a chronic skin condition by adopting a holistic approach to treatment. Prioritising self-care, seeking support from others, and being proactive in managing your health can all lead to a higher quality of life and overall well-being.
Psychological Aspects: Coping with the Emotional Toll
Living with a chronic condition such as solar urticaria can be difficult to deal with emotionally. Education and understanding, emotional expression, stress management, coping strategies, a positive outlook, and professional support are all strategies for managing the psychological aspects of the condition. Remember to prioritise self-care, seek help when necessary, and be kind to yourself as you deal with the ups and downs of living with a chronic condition.
Solar Urticaria in the Digital Age: Communities and Support
Individuals suffering from solar urticaria now have access to online communities and support networks that can offer valuable resources, information, and emotional support. Online support groups, disease-specific organisations, telemedicine and virtual support, personal blogs and websites, peer support, and empowerment are all ways to connect with communities and find help. Individuals with solar urticaria can find valuable resources, encouragement, and solidarity in their efforts to manage the condition by connecting with online communities, accessing support networks, and staying up to date on the latest developments.
Future Directions: Research and Advances in Treatment
Solar urticaria research is ongoing, to improve understanding of the condition and develop more effective treatment options. Immunotherapy, biological therapies, novel treatment approaches, personalised medicine, clinical trials, and patient-centered care are examples of potential future research directions and emerging trends. As research into solar urticaria progresses, collaboration among researchers, clinicians, industry partners, and patient communities is critical for advancing scientific understanding and improving outcomes for people living with this difficult condition.
Empowering Your Journey: Long-Term Strategies and Support for Solar Urticaria
Empowering your journey with solar urticaria entails developing long-term strategies and seeking ongoing support to effectively manage the condition and improve your overall quality of life. Some important approaches include education and awareness, sun protection, lifestyle changes, support networks, regular monitoring, advocacy, and empowerment. By implementing these long-term strategies and seeking ongoing support, you can empower yourself to effectively manage solar urticaria, reduce its impact on your life, and thrive despite the challenges presented by the condition. Remember that you are not alone, and there are resources and communities available to help you on your journey.
















