"Keratoacanthoma: Insights into a Rapidly Growing Skin Lesion" is a thorough examination of keratoacanthoma (KA), a common benign skin lesion that can resemble squamous cell cancer.
Understanding Keratoacanthoma: The Basics

"Understanding Keratoacanthoma: The Basics" is an introduction tutorial to keratoacanthoma (KA), a common skin lesion that often appears as a fast-expanding dome-shaped nodule. Here's how the blog may cover the fundamentals: clinical presentation, epidemiology, risk factors, differential diagnosis, histopathology, natural history, treatment options, prognosis, prevention, and sun protection.
Identifying Keratoacanthoma: Symptoms and Signs
Identifying Keratoacanthoma: Symptoms and Signs" is a detailed reference that teaches readers how to recognise the distinguishing signs of keratoacanthoma (KA), allowing for early diagnosis and treatment. Here's how they might outline the symptoms and signs of KA: Describe the typical symptoms and signs of keratoacanthoma, its comparison with squamous cell carcinoma (SCC), associated symptoms, risk factors, and importance of diagnosis.
Keratoacanthoma vs. Skin Cancer: Distinguishing Factors
"Distinguishing keratoacanthoma from skin cancer seeks to clarify how keratoacanthoma (KA) differs from various types of skin cancer, particularly squamous cell carcinoma (SCC). Here's how the book may explain the distinguishing factors:
-
Begin by comparing the clinical presentation of keratoacanthoma and skin cancer, emphasising the similarities and differences.
-
Rapid Growth: While both KA and SCC can grow rapidly, KA typically grows faster than SCC, reaching its maximum size in a matter of weeks or months.
-
Describe KA as a dome-shaped nodule with a central keratin-filled crater or horn. In contrast, SCC can appear as a non-healing ulcer, scaly plaque, or firm nodule with irregular borders.
-
Discuss how KA lesions can range from flesh-colored to pink, red, or brown, with a smooth or shiny surface. SCC lesions can appear red, pink, or crusty, with a rough or scaly texture.
-
It is important to note that KA lesions are most common on sun-exposed areas such as the face, ears, scalp, and dorsal hands, whereas SCC can develop on both sun-exposed and sun-free skin.
-
Mention that KA is more common in older people with a history of sun exposure, fair skin, and immunosuppression, whereas SCC can occur at any age and may be linked to chronic sun exposure, immunosuppression, and specific genetic factors.
-
Explain the histopathological characteristics of KA and SCC, such as a central keratin-filled crater surrounded by well-differentiated keratinocytes an inflammatory infiltrate in KA, and dysplastic keratinocytes invading the dermis in SCC.
-
Discuss the behaviour and prognosis of KA versus SCC, emphasising that KA has a quick development phase followed by spontaneous regression in most cases, whereas SCC is more invasive and has a higher risk of metastasis if left untreated.
-
To distinguish KA from skin cancer and ensure appropriate management, emphasise the importance of accurate diagnosis via clinical examination and, if necessary, histopathological analysis.
The Causes and Risk Factors Behind Keratoacanthoma
The causes and risk factors for keratoacanthoma shed light on the factors that influence the development of this common skin lesion. Here's how they might approach this topic:
-
Begin by defining KA as a benign skin tumour that typically appears on sun-exposed areas of the skin, with rapid growth and a dome-shaped appearance.
-
Discuss extended or excessive sun exposure as a major risk factor for KA development. Explain how ultraviolet (UV) radiation can harm the skin's DNA and contribute to the development of KA lesions, especially in people with fair skin.
-
Highlight fair skin as a major risk factor for KA. Explain that people with fair skin have less melanin, which reduces their natural protection against UV radiation and makes them more susceptible to sun damage and skin cancer, including KA.
-
Discuss age as a risk factor for KA, noting that it occurs more frequently in older people, particularly those over the age of 50. Explain how cumulative sun exposure over time increases the risk of developing KA lesions as people age.
-
Consider immunosuppression as a possible risk factor for KA. onsider immunosuppression as a possible risk factor for KA. Explain how conditions or medications that weaken the immune system, such as organ transplantation or immunosuppressive therapy, may increase the risk of developing KA lesions.
-
Mention the potential role of genetic factors in KA development. Discuss familial cases of KA and genetic syndromes associated with an increased risk of developing multiple skin lesions, including KA, such as Ferguson-Smith syndrome and Muir-Torre syndrome.
-
Discuss other environmental factors that may contribute to KA development, such as exposure to chemical carcinogens, including arsenic, coal tar, and certain industrial chemicals.
-
Mention trauma or injury to the skin as a potential trigger for KA development in some cases. Explain that trauma to the skin may disrupt normal cellular processes and contribute to the formation of KA lesions, although the exact mechanism is not well understood.
Approaching Treatment: Effective Strategies for Keratoacanthoma
"Approaching Treatment: Effective Strategies for Keratoacanthoma" is a comprehensive guide to treating keratoacanthoma (KA) lesions. Here's an outline of different treatment strategies:
-
Discuss the possibility of observation and monitoring for small, asymptomatic KA lesions with low-risk characteristics, especially in elderly patients or those with significant comorbidities. Explain the significance of regular follow-up appointments for tracking lesion progression.
-
Consider surgical excision as a primary treatment option for KA lesions, especially larger ones or those located in cosmetically sensitive areas. Discuss the surgical technique, including margin assessment and wound closure options.
-
Introduce Mohs micrographic surgery as a precise and tissue-preserving surgical technique commonly used for KA lesions with high-risk characteristics such as aggressive growth patterns, poorly defined borders, or involvement of critical anatomical structures.
-
Discuss cryotherapy as a non-surgical treatment option for KA lesions, which uses liquid nitrogen to freeze and destroy abnormal tissues. Explain its efficacy, potential side effects, and options for lesion selection and treatment duration.
-
Investigate curettage and electrodesiccation as a simple and cost-effective treatment strategy for KA lesions, which involves mechanical scraping of the lesion followed by electrocautery to destroy residual tumour cells and achieve hemostasis.
-
Discuss the use of topical treatments, such as 5-fluorouracil (5-FU) cream or imiquimod cream, as an alternative or adjuvant therapy for KA lesions, especially in patients who are not surgical candidates or prefer non-invasive options.
-
Introduce photodynamic therapy as a minimally invasive treatment for KA lesions, which involves applying a photosensitizing agent and then exposing to light to selectively destroy abnormal cells while sparing surrounding tissue.
-
Mention radiation therapy as a possible treatment for KA lesions, especially in patients who are not surgical candidates or have recurrent or extensive disease. Discuss the efficacy, potential side effects, and lesion selection criteria.
-
Investigate the role of adjuvant therapies, such as intralesional corticosteroid injections or systemic retinoids, in the treatment of KA lesions, especially in cases of incomplete excision, recurrence, or high-risk features.
Surgical Solutions: Exploring the Most Common Treatment
"Surgical Solutions: Exploring the Most Common Treatment" examines surgical approaches as the primary treatment option for keratoacanthoma (KA). Here's how they might explore this blog:
-
Surgical Technique: Describe the surgical technique for excising keratoacanthoma lesions, including the use of local anaesthesia, choosing appropriate margins, and closing the wound with sutures or other wound closure methods.
-
Margin Assessment: Explain the significance of margin assessment in ensuring complete removal of the KA lesion while reducing the risk of recurrence. Describe methods for evaluating margins, such as Mohs micrographic surgery or frozen section analysis.
-
Wound Management: Provide postoperative wound care instructions, pain management strategies, and potential complications to be aware of, such as infection or delayed wound healing.
-
Cosmetic Considerations: Discuss the cosmetic implications of surgical excision of KA lesions, especially in cosmetically sensitive areas like the face.
-
Adjuvant Therapies: Examine how adjuvant treatments, such as electrodesiccation or cryotherapy, can be used in addition to surgical excision for KA lesions. Describe how these modalities can lower the chance of recurrence and guarantee total eradication of any remaining tumour cells.
-
Patient Education and Counselling: Emphasise the importance of educating and counselling patients about the surgical procedure, expected outcomes, and potential risks and complications. Provide resources and support to help patients address their concerns and make informed decisions.
-
Follow-up Care: Discuss the importance of regular follow-up appointments to monitor the surgical site, assess wound healing, and detect any signs of recurrence. Explain the significance of long-term surveillance for KA patients, given the risk of recurrence and the possibility of future skin cancer.
Alternative Therapies: Cryotherapy, Photodynamic Treatment, and Topicals
Cryotherapy, Photodynamic Treatment, and Topicals investigate non-surgical options for treating keratoacanthoma (KA) lesions. Here's how they could discuss each alternative therapy:
-
Cryotherapy: Explain how cryotherapy works by causing cellular injury and necrosis via rapid freezing and thawing cycles, destroying KA cells. Describe the cryotherapy procedure, including the application technique, treatment duration, and after-care instructions. Discuss the efficacy of cryotherapy for KA lesions, emphasising the high cure rates and minimal scarring. Address any potential side effects, including pain, blistering, and hypopigmentation. Direct patient selection, lesion characteristics appropriate for cryotherapy, and contraindications, such as large or deeply invasive lesions.
-
Photodynamic Therapy (PDT): Explain how PDT works by specifically targeting and killing aberrant cells, such as KA cells, while protecting healthy tissue. Describe the PDT technique, including the application of the photosensitizing chemical, the incubation period, and light exposure at a certain wavelength. Discuss the efficacy of PDT for KA lesions, focusing on its high response rates and favourable cosmetic results. Address any potential adverse effects, including discomfort, erythema, and post-inflammatory hyperpigmentation. Direct patient selection, lesion features appropriate for PDT, and contraindications, such as photosensitivity diseases or porphyria.
-
Topical Treatments: Explain how topical medicines decrease DNA synthesis and induce death in aberrant cells, such as KA cells. Describe the topical agent treatment procedure, which includes application frequency, treatment duration, and response monitoring. Discuss the efficacy of topical therapies for KA lesions, emphasising their significance in causing lesion regression and preventing reoccurrence. Address any potential side effects, such as erythema, irritation, and ulceration at the application site. Guide patient selection, lesion features appropriate for topical treatment, and contraindications, such as an allergy to the active components or a damaged immune system.
Post-Treatment Care: Ensuring a Smooth Recovery
It guides how to care for the skin after a variety of keratoacanthoma (KA) treatment options. Here's how the book could outline post-treatment care strategies.
- Wound Care: Emphasise the importance of proper wound care in promoting healing and lowering the risk of complications.
-
Keep the treated area clean and dry.
-
Follow any specific wound care instructions provided by the healthcare provider.
-
To avoid infection and scarring, do not pick, scratch, or rub the treated area.
-
Use gentle cleansers and avoid harsh or abrasive skincare products until the skin is completely healed.
2. Pain Management: Discuss pain management strategies to relieve discomfort after treatment.
-
Over-the-counter pain relievers, such as acetaminophen or ibuprofen, may be recommended to manage post-procedural pain.
-
Topical analgesic creams or ointments may provide localized pain relief.
-
Cold packs or compresses can be used to relieve pain and inflammation in the treated area.
3. Monitoring for Complications: Inform patients about the signs and symptoms of potential complications, such as infection or excessive bleeding.
-
Advise patients to monitor the treated area for signs of infection, including increased pain, redness, swelling, warmth, or drainage.
-
Instruct patients to contact their healthcare provider immediately if they experience any concerning symptoms or if the treated area fails to heal as expected.
4. Sun Protection: Emphasise the importance of sun protection after treatment to avoid sun damage and reduce the risk of recurrence.
-
Advise patients to limit their sun exposure as much as possible, particularly during peak sunlight hours (10 a.m. to 4 p.m.).
-
Encourage the application of broad-spectrum sunscreen with a high sun protection factor (SPF) to the treated area and any other exposed skin.
-
Wear protective clothing, such as hats, sunglasses, and long-sleeved shirts, to shield your skin from UV rays.
5. Follow-Up Appointments: Emphasise the importance of attending follow-up appointments with your healthcare provider.
-
Schedule regular follow-up appointments to monitor the treated area, evaluate healing progress, and address any issues or complications.
-
Ensure that patients understand the significance of adhering to follow-up care to achieve the best possible outcomes and detect any signs of recurrence or complications early.
-
5. Scar Management: Use these techniques to reduce scarring and promote aesthetic healing.
-
Encourage gentle massage of the scar tissue after the wound has healed to improve circulation and prevent stiffness.
-
Use silicone-based scar gels or sheets to flatten and soften scars.
-
If necessary, discuss the possibility of using cosmetic procedures like laser therapy or microdermabrasion to improve the scar.
Beyond Treatment: Prevention and Long-Term Care

Prevention and Long-Term Care expands the discussion beyond immediate treatment options, focusing on preventive strategies and long-term care for keratoacanthoma patients. Here's how they could approach this blog.
-
Sun Protection Practices: Educate readers about the importance of sun protection in preventing KA and other skin lesions. Encourage the use of broad-spectrum sunscreen with a high SPF, applied generously and reapplied every two hours, particularly during outdoor activities. Promote the use of wide-brimmed hats, sunglasses, and protective clothes to protect the skin and eyes from UV radiation.
-
Skin Self-Examinations: Teach readers how to conduct regular skin self-examinations to detect new or changing lesions. Look for new growths, changes in the size, shape, colour, or texture of existing lesions, and any lesions that itch, bleed, or do not heal. Emphasise the significance of early diagnosis and timely evaluation by a healthcare practitioner for any abnormal skin changes.
-
Healthy Lifestyle Practices: Encourage the adoption of a healthy lifestyle, which includes a well-balanced diet rich in fruits, vegetables, and whole grains, as well as frequent exercise, to improve general health and skincare. Smoking and excessive alcohol use are discouraged since they can cause skin damage and increase the chance of developing skin lesions such as KA.
-
Regular Dermatological Check-Ups: Individuals with a history of KA or other skin malignancies should receive frequent dermatological check-ups. A dermatologist should do annual or biennial skin examinations to check for new or recurring lesions and for general skin health.
-
Medical Follow-Up Care: Encourage patients to follow the prescribed follow-up treatment plans specified by their healthcare providers, which include regular check-ups and monitoring for signs of recurrence. Identify and record any symptoms or changes that indicate recurrent KA lesions or other skin abnormalities.
-
Education and Awareness: Raising awareness of KA and its risk factors in the community and among at-risk groups. Provide educational resources, such as booklets, websites, or community seminars, to raise awareness about skin cancer prevention and early diagnosis.
-
Psychosocial Support: Recognise the psychological impact of a KA diagnosis and treatment on individuals, and provide resources like coping methods, support groups, and counselling services as needed.
Preventive Measures: Protecting Your Skin from Keratoacanthoma
Preventive measures for protecting your skin provide practical advice on how to reduce the chance of acquiring keratoacanthoma (KA) lesions. Here's how they could describe preventive tactics, including sun protection, sun-safe behaviours, skin self-examinations, healthy living habits, frequent dermatological check-ups, and education and awareness.
The Importance of Regular Dermatological Check-Ups
The importance of regular dermatological check-ups emphasises the importance of dermatologists performing routine skin examinations to maintain skin health and detect potential abnormalities, such as keratoacanthoma (KA) lesions. Here's how they could emphasise its importance:
-
Early Detection of Skin Lesions: Explain that regular dermatological check-ups allow for early detection of skin lesions, including KA, when they are most treatable. Emphasise the importance of promptly evaluating and diagnosing any suspicious or changing skin lesions to facilitate timely intervention and avoid potential complications.
-
Monitoring for Skin Cancer Risk: Discuss how dermatologists evaluate people's risk factors for skin cancer, such as sun exposure, family history, skin type, and the presence of atypical moles. Highlight the importance of regular skin examinations in monitoring high-risk individuals for signs of skin cancer, including KA, and implementing appropriate preventive or surveillance strategies.
-
Comprehensive Skin Evaluation: Describe the comprehensive nature of dermatological check-ups, which may include a head-to-toe skin examination to detect abnormalities, including KA lesions. Explain that dermatologists are trained to detect subtle changes in the skin that could be early signs of skin cancer, allowing for timely intervention and treatment.
-
Experience with Diagnosis and Treatment: Highlight dermatologists' specialised training and expertise in diagnosing and treating skin conditions, such as KA. Discuss the various diagnostic and treatment options available to dermatologists for managing KA lesions, including biopsy, surgical excision, cryotherapy, and photodynamic therapy.
-
Personalized Prevention and Management Plans: Emphasise the importance of creating personalised prevention and management plans based on individual risk factors, skin type, and lifestyle choices. Explain that dermatologists can make personalised recommendations for sun protection, skincare, and surveillance based on each patient's specific needs and situation.
-
Patient Education and Empowerment: Encourage people to take an active role in their skin health by scheduling regular dermatological check-ups and reporting any concerning skin changes right away. To reduce the risk of skin cancer, including KA, educate patients on self-examination techniques and the importance of sun protection practices.
-
Long-Term Skin Health: Regular dermatological check-ups are essential not only for early detection and treatment of skin cancer, but also for maintaining overall skin health and avoiding long-term damage. Encourage people to prioritise skin health as part of their regular healthcare routine, and to form a collaborative relationship with a reputable dermatologist for ongoing care and support.
Embracing a Healthy Skin Care Routine Post-Keratoacanthoma
Embracing a healthy skin care routine after keratoacanthoma treatment focuses on promoting skin health and preventing recurrence. Here's how they could describe a post-KA skin care routine:
-
Gentle Cleansing: Use a mild, non-abrasive cleanser to gently cleanse your skin twice a day. Avoid using harsh or abrasive cleansers that can irritate your skin.
-
Hydration: Emphasise the importance of moisturising the skin regularly to keep it hydrated and avoid dryness. To reduce irritation, use a moisturiser specifically designed for sensitive skin.
-
Sun Protection: Stress the importance of daily sun protection in preventing sun damage and lowering the risk of skin cancer recurrence. Encourage the use of broad-spectrum sunscreen with an SPF of 30 or higher, liberally applied to all exposed skin and reapplied every two hours, especially when outside.
-
Skin Barrier Repair: Consider using products containing ceramides, hyaluronic acid, and niacinamide to help repair the skin barrier and retain moisture.
-
Anti-Inflammatory Agents: Use anti-inflammatory skincare ingredients like green tea extract, licorice extract, or colloidal oatmeal to soothe and calm the skin after treatment.
-
Avoid Irritants: Avoid skincare products that contain potential irritants like fragrances, alcohol, and harsh chemicals, which can aggravate skin sensitivity.
-
Regular Follow-Up: Emphasise the importance of scheduling regular follow-up appointments with a dermatologist to monitor the skin for signs of recurrence or new lesions.
-
Skin Self-Examination: Educate people on how to perform regular skin self-examinations to check for changes in existing lesions or the development of new ones. Encourage them to immediately report any concerning changes to their dermatologist.
-
Healthy Lifestyle: To promote overall skin health, adopt a healthy lifestyle that includes a well-balanced diet, regular exercise, stress management, and adequate sleep.
-
Avoid Smoking and Excessive Alcohol: Smoking and excessive alcohol consumption are discouraged because they can cause skin damage and increase the risk of developing skin lesions such as KA.
-
Psychological Support: Recognise the psychological impact of a KA diagnosis and treatment, and offer resources for coping strategies and support groups as needed.
-
Skin Cancer Awareness: Raise awareness among family and friends about the importance of skin cancer prevention and early detection, and encourage them to practise sun safety and get regular skin exams.
Following KA, people can preserve overall wellbeing, promote skin health, and reduce the chance of recurrence by adopting a good skin care regimen.
The Future of Keratoacanthoma Care: Advances and Innovations
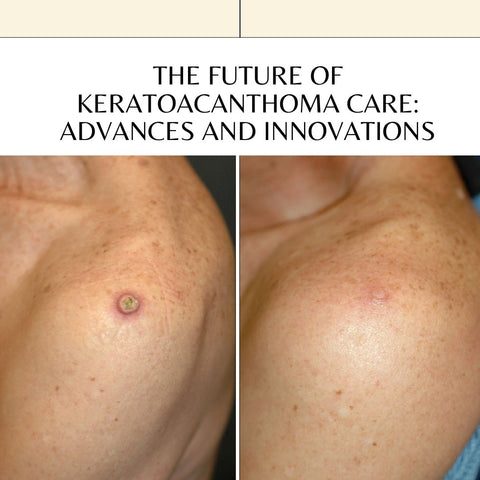
The future of keratoacanthoma care looks at prospective advances in the diagnosis, treatment, and management of keratoacanthoma (KA) lesions. Here's how they may talk about future directions in KA care, including precision medicine and molecular diagnostics, targeted medicines, immunotherapy, topical treatments, minimally invasive therapies, artificial intelligence and digital health, regenerative medicine, and patient-centered care.
















