Milia are tiny, white pimples that occur on the skin, most commonly on the face. They originate when keratin, a skin protein, becomes trapped beneath the surface and forms microscopic cysts. While milia are usually harmless, many people seek treatment for cosmetic reasons. It's critical to remember that milia should never be squeezed or picked at home because it can cause skin irritation, infection, or scarring. If you're confused about how to treat milia or if they're causing you concern, speak with a dermatologist or skin care professional who can offer personalized guidance and prescribe appropriate treatment choices based on your individual case. Additionally, preventative measures like using non-comedogenic products, exfoliating frequently, and maintaining good skin care hygiene can lessen the possibility of milia development.
Understanding Milia: Causes, Characteristics, and Misconceptions

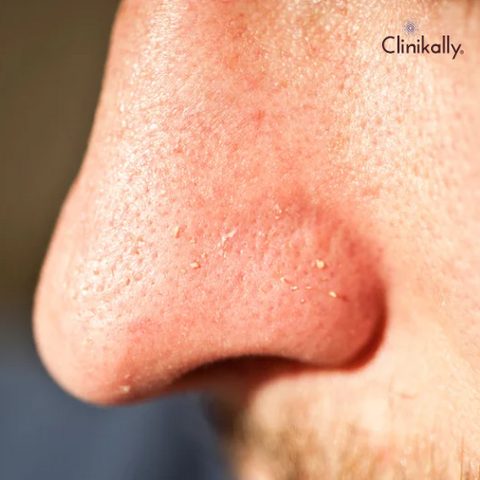
Milia are tiny, white, or yellowish pimples on the skin that usually arise on the face. Here's a closer look at the causes, symptoms, and frequent myths about milia:
Causes: Keratin build-up, skin damage or trauma, and clogged sweat ducts are the causes of milia.
Characteristics of Milia:
-
Appearance: Milia are small, dome-shaped bumps that are usually white or yellowish in color. They have a smooth texture and are typically 1 to 2 millimetres in size.
-
Location: Milia are frequently found on the face, especially close to the eyes, cheeks, and nose. They can, however, also show up elsewhere on the body.
-
Painless: Milia are typically painless and do not bother you unless they swell up or irritate you.
Misconceptions about Milia:
-
Milia are bumps or acne: Milia are frequently confused with bumps or acne, but they are not the same. Milia are skin-deep cysts, as opposed to the inflammation and clogged hair follicles associated with acne.
-
Milia are simple to pop or squeeze: Milia should not be squeezed or popped at home, in contrast to blackheads or pimples. Self-extraction of milia can damage skin, inflame it, and possibly leave scars. To ensure safe and successful removal, it is best to seek professional assistance.
-
Milia spread easily: Milia do not spread easily. They can affect people of all ages and skin types, and they are benign skin conditions.
-
Milia will disappear on their own: While some milia may resolve spontaneously over time, many persist without treatment. If milia are bothersome or affecting your self-confidence, professional intervention may be necessary.
If you have concerns about milia or want them removed, you should see a dermatologist or skin care professional. Based on the features of your milia and your skin type, they can provide an accurate diagnosis and treatment alternatives.
Unveiling the Mystery: What Exactly is Milia?
It frequently develop on the skin. These cysts are usually tiny and spherical, with a white or yellowish color. Milia are most commonly found on the face, notably around the eyes, cheeks, and nose, but they can arise elsewhere on the body. Milia form when keratin, a skin protein, becomes stuck under the surface. They are most typically found in infants and are known as neonatal milia. Milia in neonates normally goes away on its own within a few weeks or months. Milia can, however, occur in both children and adults.
Milia primarily comes in two different forms:
-
Primary Milia: These can affect people of all ages and are the most prevalent type of milia. Keratin gets trapped beneath the skin's surface, frequently as a result of the skin's inability to properly exfoliate dead cells, and this leads to the development of primary milia. Although the precise cause of primary milia is not fully understood, they can be linked to elements like sun damage, specific skin conditions, or skin trauma.
-
Secondary Milia: Secondary milia can appear after skin trauma or damage, including burns, blistering wounds, or specific skin treatments. They are also linked to genetic disorders like Gardner syndrome as well as skin conditions like bullous pemphigoid and porphyria cutanea tarda.
Milia are often painless and innocuous. Many people who seek treatment for their looks regard it as a cosmetic concern. While milia can sometimes dissolve on its own, professional intervention may be required to remove chronic or irritating milia. It's critical to remember that milia should never be squeezed or picked at home because it can cause skin irritation, infection, or scarring. If you have milia concerns, it is best to visit with a dermatologist or skincare professional who can provide a proper diagnosis and treatment choices based on your unique case.
Common Causes: Identifying the Triggers Behind Milia Formation
There are numerous causes for the development of milia. Some of the causes of milia development include the ones listed below:
-
Building up keratin: Keratin, a protein found in the skin's outermost layer, is the major cause of milia. Milia occurs when keratin becomes trapped beneath the skin's surface and forms tiny cysts.
-
Skin damage or trauma: Skin damage or trauma, such as burns, blistering wounds, or even specific skin treatments like dermabrasion or laser resurfacing, can result in the development of milia. The trauma interferes with the natural process of dead skin cells being shed, resulting in their becoming trapped and forming cysts.
-
Excessive sun exposure: Milia can develop as a result of prolonged sun exposure without adequate protection. The outer layer of the skin can become thicker as a result of sun damage, making it more difficult for dead skin cells to be properly shed. This can result in a build-up of keratin and the emergence of milia.
-
Use of occlusive or heavy skincare products: The use of certain skincare products, particularly occlusive or heavy moisturizers or creams, has the potential to promote the development of milia. These products might develop a barrier on the skin's surface, which would stop the natural shedding of dead skin cells and result in keratin build-up.
-
Genetic predisposition: Milia development may be genetically predisposed in some people. Your likelihood of developing milia may increase if the condition runs in your family.
-
Use of comedogenic cosmetics: Products with the comedogenic label have the potential to clog pores and cause milia to form. Examples include heavy foundations and creams. In order to reduce the risk, it is advised to select products that are non-comedogenic or oil-free.
It is important to remember that milia can affect people of all ages and skin types, including infants, kids, and adults. While milia can be an aesthetic issue, they are typically painless and do not need medical attention unless they are severely obstructing vision (in the case of milia near the eyes) or causing significant discomfort. The best course of action, if you have persistent or bothersome milia, is to speak with a dermatologist or skincare expert who can make a proper diagnosis and suggest suitable treatments based on the underlying cause and your unique situation.
Dispelling Myths: Separating Facts from Fiction About Milia
There are numerous myths and misconceptions surrounding milia, just like many other skin conditions. Let us separate fact from fiction and debunk a few milia myths:
-
Myth 1: Milia are an acne-like condition. Fact: Milia are frequently confused with acne, but they are not the same thing. Acne is an inflammation of the hair follicles, whereas milia are cysts formed beneath the skin's surface from trapped keratin. The causes, treatments, and underlying mechanisms of milia and acne differ.
-
Myth 2: Milia are contagious. Fact: Milia are not contagious. They are not caused by germs, viruses, or other external factors that can be passed from person to person. Milia are caused by keratin build-up or skin trauma and do not spread from person to person.
-
Myth 3: Squeezing or popping milia will make them disappear. Fact: It is not advised to squeeze or try to pop milia at home. Milia are challenging to remove because they do not have an opening to the skin's surface like blackheads or pimples do. Squeezing or popping milia can harm the skin, cause inflammation, and possibly leave scars. If milia need to be extracted, it is best to seek professional help.
-
Myth 4: Milia are only observed in young children and elderly people. Fact: Milia can affect people of any age, though they are most frequently found in older adults and newborns (neonatal milia). The most typical type, primary milia, can appear in people of any age, including kids, teenagers, and young adults.
-
Myth 5: Bad hygiene is the root of milia. Fact: Poor hygiene or cleanliness are not what cause milia. Keratin being stuck beneath the skin's surface is a common reason. Maintaining proper skin care hygiene, which includes routine cleaning and exfoliation, can help to avoid the accumulation of dead skin cells and reduce the probability of getting milia.
-
Myth 6: Sun exposure can cure milia. Fact: Sunlight does not cure milia. While some people may notice a temporary improvement in their milia as a result of sun-induced skin exfoliation, excessive sun exposure without adequate protection can cause other skin problems and potentially worsen milia in the long run. To keep your skin healthy overall, it is critical to use sunscreen frequently and protect your skin from the sun.
If you have milia problems or want them eliminated, you should see a dermatologist or skin care professional. They can provide an accurate diagnosis, address your unique situation, and recommend appropriate treatment options based on your needs and preferences.
Expert Advice on Milia Treatment: Tips, Techniques, and Remedies

When it comes to treating milia, it's critical to proceed with caution and seek professional help if necessary. Here are some advice, tactics, and cures for dealing with milia:
-
Professional extraction: Consult a dermatologist or skincare specialist who can perform a safe extraction if you have chronic or irritating milia. They will use sterile instruments and techniques to remove the milia with minimal injury to the surrounding skin.
-
Chemical peels: Chemical peels have the potential to help remove milia by encouraging the shedding of dead skin cells and exfoliating the skin. To choose the right kind and strength of chemical peel for your skin type and to make sure it is done safely, you must, however, speak with a professional.
-
Retinoids: Topical retinoid creams or gels with active ingredients such as tretinoin or adapalene may aid in accelerating skin cell turnover and minimizing keratin buildup. These products may require a prescription and should be used under the direction of a dermatologist.
-
Microdermabrasion: This method of exfoliation uses a tool to delicately scrape off the top layer of dead skin cells, possibly assisting in the treatment of milia. This procedure, however, should be performed by a trained professional to avoid complications.
-
Home remedies: While there is little scientific evidence to support the effectiveness of home remedies for milia, some people report success with particular methods. These include applying a warm compress to the affected area to help soften the skin and encourage milia removal or using gentle exfoliants like baking soda and water. However, it is critical to proceed with caution and stop using any home remedy if it irritates you or makes your condition worse.
-
Prevention: It may be advantageous to take measures to stop the development of milia. This entails using non-comedogenic or oil-free skincare items, staying away from thick or occlusive creams, shielding your skin from too much sun exposure, and routinely exfoliating to keep the skin's surface clear.
To reduce the risk of infection or scarring, it is crucial to note that professional milia removal techniques should be used. It is best to seek advice from a dermatologist or skincare expert if your milia are bothersome or persistent so that they can assess your unique situation and suggest the best course of action.
Treating Milia: Dermatologist-Recommended Techniques and Products
It is critical to remember that expert assistance from a dermatologist is required for an accurate diagnosis and personalized treatment plan. Dermatologists may recommend the following techniques and products:
-
Professional extraction: Dermatologists are able to carefully remove the milia using sterile tools during a procedure known as milia extraction. This is frequently regarded as the most efficient and secure way to treat milia.
-
Topical retinoids: Dermatologists may recommend topical retinoid creams or gels with tretinoin or adapalene as active ingredients. These products can facilitate exfoliation, hasten skin cell turnover, and stop the growth of new milia.
-
Chemical peels: A chemical solution is applied to the skin during a chemical peel to help exfoliate the top layer of the skin and improve the appearance of milia. This procedure should only be performed by a trained professional.
-
Cryotherapy: Dermatologists may use liquid nitrogen to freeze the milia in some cases. This technique can aid in the destruction of milia and their removal.
-
Microdermabrasion: Dermatologists may recommend microdermabrasion, a procedure that uses a device to gently exfoliate the skin's outer layer. This can improve the appearance of milia by encouraging natural shedding.
-
Exfoliants with a prescription: Dermatologists may prescribe prescription-strength exfoliants like alpha hydroxy acids (AHAs) or beta hydroxy acids (BHAs) to help remove dead skin cells and prevent milia formation.
-
Proper skincare regimen: To prevent the build-up of dead skin cells and lower the risk of milia formation, dermatologists may advise patients to adhere to a gentle skincare routine that includes frequent cleansing and exfoliation.
A dermatologist should be consulted for a precise diagnosis and a customized treatment plan for your particular case of milia. They will advise you on the procedures and products that are best for you after taking into account your skin type, medical history, and the severity of the milia.
Natural Remedies: Harnessing Nature's Solutions for Milia Treatment
While professional therapy for milia is suggested, some natural therapies may be used in conjunction with or as a supplement to professional care. It's crucial to remember that the efficacy of natural milia therapies varies, and individual results may vary. Here are a few natural therapies that some people have found to be beneficial:
-
Honey: Honey has antibacterial and exfoliating properties that are natural. A small amount of raw honey applied to the affected area and left on for a few minutes before rinsing off may help soften the skin and promote natural milia removal.
-
Tea tree oil: Tea tree oil has antibacterial and anti-inflammatory properties. Applying tea tree oil diluted with a carrier oil, such as coconut or jojoba oil, to milia spots may help reduce inflammation and potentially promote resolution. However, a patch test should be performed first to rule out any skin sensitivity or irritation.
-
Apple cider vinegar: Apple cider vinegar is well-known for its exfoliating properties. Using a cotton pad to apply a diluted solution of apple cider vinegar and water to the affected area may help remove dead skin cells and potentially aid in milia resolution. However, be cautious because undiluted apple cider vinegar may irritate the skin.
-
Aloe vera: The soothing and moisturizing qualities of aloe vera gel are well known. Applying fresh aloe vera gel to the milia spots may hydrate the skin and possibly encourage healing. Look for pure aloe vera extract or gel made from the plant's leaves.
-
Gentle exfoliation and steam: Steam can help soften skin and widen pores. Milia can be removed naturally by gently steaming the face and then exfoliating the area with a soft, clean cloth. Avoid rubbing vigorously because it can irritate your skin.
-
Healthy eating and hydration: A balanced diet full of fruits, vegetables, and antioxidants can improve the health of your skin on the whole. Even though there is not any concrete evidence connecting particular dietary changes to the disappearance of milia, leading a healthy lifestyle may promote the skin's inherent healing abilities.
The Role of Exfoliation: How Proper Exfoliating Benefits Milia-Prone Skin
Exfoliation is important in the management of milia-prone skin since it helps to remove dead skin cells, unclog pores, and encourage the natural shedding of milia. Exfoliation can help milia-prone skin in the following ways:
-
Removal of dead skin cells: Milia can form when dead skin cells get sucked up beneath the skin's surface, creating tiny cysts. Exfoliation on a regular basis helps to get rid of these dead skin cells, preventing their buildup and lowering the chance of developing milia.
-
Unclogging pores: Milia can happen when pores get blocked with dirt, oil, or keratin that has been trapped. By removing the build-up of these substances, exfoliation helps to open up pores, allowing the skin to breathe and preventing milia from forming.
-
Promoting cell turnover: Exfoliation helps stimulate the skin's natural cell turnover process, which is important for maintaining healthy skin. Exfoliation can help prevent the build-up of keratin and lessen the risk of milia formation by accelerating the shedding of old skin cells and promoting the production of new ones.
-
Smoothing skin texture: Milia can cause rough and uneven skin texture. Regular exfoliation can help smooth the skin's surface by removing dead skin cells and promoting a more even skin tone and texture.
When treating milia-prone skin, use mild exfoliation procedures and avoid abrasive or harsh scrubs that may irritate or injure the skin. The following tips will assist you in properly exfoliating. Choose a gentle exfoliant, stick to a schedule, moisturize, and protect your skin. If you have recurrent or severe milia, see a dermatologist who can provide you with personalized advice and assistance on the best exfoliating methods for your skin type and condition.
Milia Treatment: Professional Procedures and Special Considerations
Dermatologists or skin care specialists may recommend professional procedures for more difficult or persistent cases of milia. These methods effectively remove milia while causing the least amount of scarring. The following are a few expert milia treatment techniques:
-
Milia extraction: This common procedure involves carefully removing the milia with a sterile needle or blade by a dermatologist or esthetician. The procedure entails making a very small skin incision and carefully extracting the milia's contents.
-
Electrocautery: A small electric current is used to burn or cauterize the milia during this procedure. This helps to break down the milia and promotes their removal. Only a trained professional should use electrocautery.
-
Chemical peels: Dermatologists may recommend chemical peels to treat milia. Chemical peels involve the application of a chemical solution to the skin, which exfoliates and removes the skin's top layer. This can improve the appearance of milia by encouraging natural shedding.
-
Microdermabrasion: Microdermabrasion is a skin exfoliation procedure that uses a device to gently exfoliate the skin's outer layer. It can help improve the appearance of milia by encouraging natural removal.
-
Laser therapy: Dermatologists may use laser therapy to treat milia in some cases. The milia can be targeted and destroyed with laser treatment, resulting in their removal. Depending on the specifics of the milia and the patient's skin type, various lasers may be employed.
These medical procedures should only be carried out by licensed professionals in order to ensure safety and lower the likelihood of complications. Important factors to take into account include skin preparation, post-procedure care, individualized treatment, and possible side effects. To identify the best treatment option for your unique instance of milia, speak with a dermatologist. They will examine your skin and make personalized recommendations for the most effective and safe treatment alternatives.
Professional Milia Removal: What to Expect and When to Seek Help
When you choose professional milia removal, it's important to understand what to expect during the operation and when you should seek assistance. Here's a rundown of what to expect and when to see a dermatologist:
-
Procedure process: Your dermatologist's expertise will establish the specific process for milia removal. Common techniques include milia extraction, electrocautery, chemical peels, microdermabrasion, and laser treatment. The procedure is often performed in the office of a dermatologist or a skincare clinic.
-
Preparation: Your dermatologist will tell you how to get ready for the procedure. This may include avoiding certain skincare products, medications, or activities that could affect the outcome or increase the risk of complications.
-
Numbing or anaesthesia: A topical anaesthetic or numbing cream may be applied to the area being treated, depending on the procedure and your pain tolerance. This reduces discomfort during the procedure.
-
Procedure time: The length of the procedure depends on the number and size of the milia being treated. Simple extractions may only take a few minutes, whereas more involved treatments such as chemical peels or laser therapy may necessitate longer sessions.
-
Sensations during the procedure: Depending on the technique used, you may feel slight pressure or a mild stinging sensation during the procedure. If you are experiencing any discomfort, it is critical that you communicate with your dermatologist.
-
Aftercare instructions: Your dermatologist will provide detailed aftercare instructions. This may include advice on how to cleanse, moisturize, and protect the treated area. Following these instructions is critical to reducing the risk of complications and promoting proper healing.
When to seek help:
-
Persistence or recurrence: If you notice that milia persists or recurs after professional removal, you should consult your dermatologist. This could point to an underlying problem that needs to be addressed.
-
Complications: Seek immediate medical attention if you experience severe pain, excessive bleeding, signs of infection (such as redness, swelling, warmth, or pus), or any other unexpected reactions following the procedure.
-
Unsatisfactory results: Consult your dermatologist if you are dissatisfied with the milia removal results or have concerns about scarring or skin texture. They can assess the results and provide additional guidance or recommend additional treatments if necessary.
-
New or changing moles or lesions: If you notice new or changing moles or lesions on your skin, you should consult a dermatologist. They can determine whether additional investigation or treatment is required.
Tackling Stubborn Milia: Strategies for Dealing with Resistant Cases
Dealing with stubborn or resistant cases of milia can be difficult, but there are some strategies you can try to help. Here are some approaches to think about:
-
Patience and observation: Milia can sometimes resolve on their own over time without the need for treatment. It is important to be patient and keep an eye on the milia to see if they go away. However, if they persist or worsen, you may need to seek alternative treatment.
-
Gentle exfoliation: Exfoliating your skin on a regular basis can help prevent the build up of dead skin cells and promote the natural shedding of milia. Use gentle exfoliating products or techniques that are appropriate for your skin type. Avoid abrasive or harsh scrubbing methods that may irritate the skin.
-
Retinoids: Topical retinoids, such as tretinoin or adapalene, can be effective in treating milia. These medications aid in cell turnover and the prevention of new milia formation. They should, however, be used under the supervision of a dermatologist because they can cause skin irritation and dryness.
-
Professional treatments: In difficult cases, dermatologists or skin care professionals may be required to perform professional procedures. These can include milia extraction, electrocautery, chemical peels, microdermabrasion, and laser therapy. Your dermatologist will recommend the best treatment option for you based on the characteristics of your milia and your skin type.
-
Needle extraction at home: You can try gentle milia extraction at home using a sterilized needle or pin if you're comfortable and familiar with skincare treatments. To minimize infection and scarring, however, it is critical to exercise caution and maintain adequate cleanliness. The usual recommendation is to have a professional perform extractions to reduce risks.
-
Avoid picking or squeezing: Resist the urge to pick or squeeze milia, as this can cause skin damage, inflammation, and scarring. Picking can also introduce bacteria into the environment, increasing the risk of infection.
-
Seek professional help: If your milia persist or you are unsure how to proceed, you should see a dermatologist. They can evaluate your specific case, determine the underlying cause of the milia, and recommend treatment options that are tailored to your specific needs.
It is important to note that prevention is essential in the treatment of milia. Maintaining a consistent skincare routine, utilizing non-comedogenic products, and keeping the skin clean and moisturized can all aid in the prevention of fresh milia production. Keep in mind that everyone's skin is different, and what works for one person may not work for another. Consultation with a dermatologist is essential for receiving personalized advice and guidance for dealing with obstinate milia. Based on your specific circumstances, they can recommend the best treatment alternatives for you.
Prevention and Maintenance: Building a Skincare Routine for Milia-Prone Skin

If you are prone to developing milia, a regular skincare routine will help prevent their production and keep your skin healthy. Here are some pointers for developing a skincare regimen for milia-prone skin:
-
Gently cleanse: To remove dirt, oil, and impurities from your skin, use a gentle, non-comedogenic cleanser. Avoid using abrasive cleansers or vigorous rubbing because these actions can irritate the skin and possibly lead to the development of milia.
-
Exfoliate frequently: Exfoliating frequently can help prevent the accumulation of dead skin cells that can lead to milia. However, use caution when using exfoliating tools or methods to prevent over-exfoliation, which can harm the skin. Alpha-hydroxy acids (AHAs) or beta-hydroxy acids (BHAs) are mild chemical exfoliants that can be used as directed.
-
Use the right amount of moisturizer: To keep your skin hydrated without clogging your pores, use a non-comedogenic, lightweight moisturizer. To reduce the chance of milia development, look for moisturizers marked "oil-free" or "non-comedogenic." Moisturizing can prevent excessive dryness, which can worsen milia and interfere with the skin's natural barrier function.
-
Sun protection: It is important for overall skin health to protect your skin from the sun. Apply broad-spectrum sunscreen every day, even on overcast days, with an SPF of 30 or higher. Proper sun protection is crucial because exposure to the sun can harm the skin and increase the risk of the development of milia.
-
Avoid using bulky or occlusive products: The development of milia may be influenced by skincare products that are thick, heavy, or greasy. Choose breathable formulations that are lightweight. To lessen the chance of pore clogging, look for products marked "non-comedogenic," "oil-free," or "gel-based."
-
Avoid using too many oil-based cosmetics: Oil-based makeup and skincare products are more likely to clog pores and contribute to milia. Consider using foundations, primers, and moisturizers that are oil-free or water-based.
-
Cleanse makeup brushes and tools: Regularly clean your makeup brushes and tools to remove any buildup of product, dirt, or bacteria that can contribute to skin issues. The risk of milia formation can be decreased by using clean brushes and tools to prevent clogged pores.
-
Be wary of eye creams: Eye creams and heavy moisturizers used around the eyes can sometimes contribute to the formation of milia. If you are prone to milia in that area, use lighter eye creams or avoid them entirely. If you must use an eye cream, use it sparingly and keep it away from the lash line.
-
Avoid excessive touching or rubbing: Avoid excessively touching or rubbing your skin, as this can irritate the skin and contribute to the formation of milia. When applying skincare products or removing makeup, use caution.
-
Regular professional skin examinations: Take into account setting up routine appointments with a dermatologist or other skincare expert who can assess your skin's condition and offer tailored advice for milia prevention and management.
Milia Prevention: Lifestyle Factors and Skincare Habits to Consider
Aside from a regular skincare routine, several lifestyle variables and skincare practices might help prevent milia. Here are some things to keep in mind:
-
Hygiene and cleanliness: Keep your hands clean by washing them before touching your face. This reduces the transfer of dirt, bacteria, and oils to your skin, which can contribute to the formation of milia.
-
Avoid heavy occlusive products: Heavy creams, oils, and occlusive skincare products can trap dead skin cells and sebum, resulting in clogged pores and the formation of milia. Choose non-comedogenic, lightweight products that will not clog your pores.
-
Cleanse after sweating: If you exercise or spend time in hot and humid environments, make sure to cleanse your face afterwards. Sweat can combine with oil and debris on your skin, potentially clogging pores and contributing to the formation of milia.
-
Avoid excessive sun exposure: Excessive exposure to the sun's harmful ultraviolet (UV) rays can cause skin damage and the formation of milia. Protect your skin by wearing sunscreen, seeking shade, and wearing protective clothing, especially during peak sun hours.
-
Be mindful of your hair and hair products: Avoid allowing heavy styling gels or oils to come into contact with your face. These products have the potential to transfer to the skin and contribute to the formation of milia. Additionally, avoid using oily hair care products near the forehead or temples, as the oils can migrate to the skin and potentially clog pores.
-
Watch what you eat: Although the connection between diet and milia is not well established, eating a balanced diet and limiting your intake of greasy or oily foods may help to improve your skin's overall health.
-
Stop squeezing or picking at the milia: Refuse to give in to the urge to do so. This may result in skin irritability, inflammation, and even scarring. A safer course of action is to let milia resolve naturally or to seek professional assistance for removal.
-
Regular skin checks: Make appointments with a dermatologist or other skincare specialist on a regular basis. They can offer individualized advice while also assisting in the identification of any underlying skin conditions or issues that might contribute to the development of milia.
Avoiding Milia Around the Eyes: Gentle Care for Delicate Skin
The skin surrounding the eyes is thin and susceptible to milia development. To avoid milia in this area, extra care and a delicate skincare routine are required. Here are some pointers for caring for the delicate skin around the eyes:
-
Use non-irritating, mild eye cleaners: Opt for a cleanser that is designed especially for the eye area. Choose items that have undergone ophthalmological examination and are fragrance-free. Avoid using harsh cleansers or typical facial cleansers on delicate eye skin because they might be too harsh.
-
Use an eye cream with caution: Use eye cream sparingly and choose lightweight, non-comedogenic formulations. Apply a small amount of product to the orbital bone area around the eyes with your ring finger and gently tap it in. Applying the cream too close to the lash line may cause hair follicles to become clogged and contribute to milia formation.
-
Protect with sunglasses: Use UV-protective sunglasses to shield the sensitive eye area from the sun's harmful rays. The skin must be protected from UV exposure because sun damage may result in the development of milia.
-
Avert using heavy eye makeup near your eyes: Products with a high-fat content, such as creamy eyeshadows and thick eyeliners, may clog your pores and cause milia to develop. Choose makeup that is non-oily, lightweight, and less likely to clog pores.
-
Gently remove makeup: When removing eye makeup, use a gentle, oil-free makeup remover. Keep your hands off the sensitive skin around your eyes, as doing so can irritate it and possibly cause milia.
-
Hydrate the eye area: To hydrate the delicate skin around the eyes, apply a light, hydrating eye gel or serum. Look for non-comedogenic products that are specially formulated for the eye area.
-
Avoid rubbing or touching your eyes excessively: Excessive rubbing or touching your eyes may irritate the skin and cause milia to develop. When applying or adjusting eye makeup, use a gentle touch rather than rubbing it in.
-
Regularly clean eye makeup brushes: Clean your eye makeup brushes regularly to remove any build-up of product, dirt, or bacteria. This helps to prevent clogged pores and lowers the likelihood of milia formation.
-
Seek professional assistance: Consult a physician or skin care specialist if you have recurring milia around the eyes or if you are unsure how to properly care for sensitive skin. They can offer tailored advice and recommend appropriate items and treatments.
Patience and Persistence: Navigating the Journey to Milia-Free Skin
Milia can be obstinate and take time to resolve, so achieving milia-free skin requires patience and commitment. Here are some pointers to help you on your way to milia-free skin:
-
Maintain consistency in your skincare regimen: Maintain a consistent skincare regimen that includes gentle cleansing, exfoliation, moisturization, and sun protection. In dealing with milia and preventing its recurrence, consistency is essential.
-
Avoid picking or squeezing milia: It may be tempting to try to remove milia on your own, but doing so can cause skin damage and scarring. Instead, focus on gentle skin care practices and seek the advice of a dermatologist or skin care professional for milia removal techniques.
-
Consider professional treatments: If you have persistent milia or milia that is causing significant concern, professional treatment may be beneficial. Extraction, chemical peels, microdermabrasion, and laser treatments can be performed by dermatologists and skin care professionals to help remove milia safely and effectively.
-
Give it some time: Milia can be difficult to resolve, particularly if they are deeply embedded. Be patient and consistent with your skincare routine, as noticeable improvement may take several weeks or even months.
-
Adjust your skincare products: If you suspect that certain skincare products are contributing to milia formation, consider switching to lighter, non-comedogenic formulations. Avoid using heavy creams or oily products, which can clog the pores and cause milia.
-
Maintain a balanced diet and stay hydrated: Proper hydration and a healthy diet can help with overall skin health. To support skin health, drink plenty of water and eat a well-balanced diet rich in fruits, vegetables, and nutrients.
-
Manage underlying skin conditions: Addressing underlying skin conditions such as dryness, inflammation, or acne can help prevent the development of milia. If you have any underlying skin concerns, consult a dermatologist to develop a comprehensive treatment plan.
-
Sun protection: Sun exposure can contribute to skin damage and potentially worsen milia. Wear sunscreen every day, seek shade when the sun is at its hottest, and cover up with protective clothing to reduce sun exposure.
-
Seek professional advice: Speak with a dermatologist or skincare expert if you are dealing with persistent milia or have questions about your skincare regimen. They can evaluate your skin's health, make tailored recommendations, and walk you through the process of getting rid of milia.
Remember that everyone's skin is different, and what works for one person may not work for another. Be patient, adjust your skincare routine as needed, and seek professional help if needed. You may walk the path to milia-free skin with time, consistency, and the appropriate attitude.
















